Quick Anatomy Overview of the Knee
The knee joint involves 4 bones:
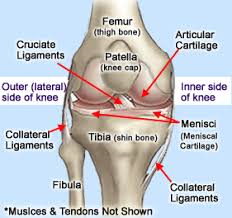
- Femur
- Tibia
- Fibula
- Patella
There are four main ligaments that stabilize the knee:
- Anterior Cruciate Ligament (ACL)
- Posterior Cruciate Ligament (PCL)
- Medial Collateral Ligament (MCL)
- Lateral Collateral Ligament (LCL)
This article will focus on the ACL. The ACL is located in the center of the knee along with the PCL. The ACL is responsible for stabilizing knee rotation that occurs during cutting and pivoting activities. It is responsible for stabilizing the knee joint in two ways:

1. The ligament acts as a passive restraint to excessive movement through its connection to the tibia and the femur.
2. ACL has mechanically sensitive nerve receptors, called proprioceptors, which sense the position of the joint.
How Does the ACL Get Injured?
- ACL injury usually occurs without contact from another player (non-contact injury)
- most common form of non-contact injury is a deceleration injury
- an athlete often plants their foot on the ground to cut or change directions and the ACL cannot withstand the force
- ACL also can be torn if the knee is forcefully hyperextended while landing from a jump
Signs & Symptoms of an ACL Tear
- ACL injury causes pain and a excessive swelling in the knee
- on occasion people say they felt or heard a “pop” in the knee
- often hard to walk after an ACL tear
- usually hard to bend and straighten the knee all the way after the injury
- after swelling goes down, people may feel like the knee “gives out”
Evaluation to Confirm an ACL Tear
- orthopedic evaluation
- Lachman’s Test
- Anterior drawer
- Pivot shift test
- MRI can visualize soft tissue and is a relatively accurate test in predicting an ACL tear

- KT-100 is a device that measures the laxity or looseness
- diagnostic arthroscopy
Treatment
Rehabilitative efforts are attempted for ACL injuries prior to surgical intervention. ACL rehabiltation focuses on improving the athlete’s proprioception and stabilization, soft tissue therapy, and physical therapy modalities. If the instability continues, the athlete should undergo surgical reconstruction of the ligament to return to activity. A potential complication to not surgically repairing a torn ACL could be degeneration of the knee joint due to instability.
Surgical Options
ACL surgery is common, but not correctly, referred to as an ACL repair. A repair implies that you can fix something that is broken. If an ACL is completely torn, the ends of the torn ligament will not heal back together, even if the torn ends were sewn together.
What does work well, is to remove the torn ends of the ACL and replace the ligament with a different structure — called an ACL graft. A graft is a tissue that is moved from one location to another. When the source of the graft is from the individual having surgery, it is called an autograft. When the source is from a donor (cadaver), it is called an allograft.
To secure the grafted ligament into the position of the normal ACL, tunnels are made of the shin bone (tibia) and thigh bone (femur), and the graft is passed through these tunnels to reconstruct the ligament.
Patellar Tendon Autograft
The patellar tendon connects the kneecap (patella) to the shin bone (tibia). When a patellar tendon graft is selected, the central 1/3 of the patellar tendon is removed along with a block of bone at the sites of attachment on the patella and tibia.
- Advantages: Many surgeons prefer the patellar tendon graft because it closely resembles the torn ACL. The length of the patellar tendon is about the same as the ACL, and the bone ends of the graft can be placed into the bone where the ACL attaches. This allows for “bone to bone” healing, something many surgeons consider to be stronger than any other healing method.
- Disadvantages: When the patellar tendon graft is taken, a segment of bone is removed from the kneecap, and about 1/3 of the tendon is removed. There is a risk of patellar fracture or tendon tear following this surgery. Also, the most common problem following this surgery is anterior knee pain. In fact, patients sometimes say they have pain when kneeling, even years after the surgery.
Hamstring Tendon Autograft
When the hamstring tendons are used in ACL surgery, two of the tendons of these muscles are removed, and “bundled” together to create a new ACL.
- Advantages: The most common problem following ACL surgery using the patellar tendon is a pain over the front of the knee. Some of this pain is known to be due to the graft and bone that is removed. This is not a problem when using the hamstring tendon. The incision to obtain the graft is smaller, and the pain both in the immediate postoperative period and in the future is thought to be less.
- Disadvantages: The primary problem with these grafts is the fixation of the graft in the bone tunnels. When the patellar tendon is used, the bone ends heal to the bone tunnels (“bone to bone” healing). With the hamstring grafts, a longer period of time is necessary for the graft to become rigid. Therefore, people with hamstring grafts are often protected for a longer period of time while the graft heals.
Allograft (Donor Tissue)
Allograft is most commonly used for recreational athletes (as opposed to competitive athletes), or patients who are undergoing revision ACL surgery (when an ACL reconstruction fails). Studies have clearly shown that allograft (donor tissue from a cadaver) is not as strong as a patient’s own tissue (autograft). For many patients, however, the strength of the reconstructed ACL using an allograft is sufficient for their demands. Therefore, this may be an excellent option for patients not planning to participate in highly competitive sports that involve excessive torque at the knee.
- Advantages: Performing ACL surgery using allograft allows for decreased operative time, no need to remove other tissue to use for the graft, smaller incisions, and less post-operative pain. Furthermore, if the graft were to fail, revision surgery could be performed using either the patellar tendon or hamstring grafts.
- Disadvantages: The process of graft preparation (freeze-drying), kills the living cells and decreases the strength of the tissue. There is also the concern of disease transmission. While sterilization and graft preparation minimizes this risk, it does not eliminate it entirely.
How to Choose an ACL Graft?
Many surgeons have a preferred type of graft for different reasons. The strength of patellar tendon and hamstring grafts are essentially equal. There is no right answer as to which is best, at least not one that has been proven in scientific studies.
The strength of allograft tissue is less than the other grafts, but the strength of both the patellar tendon and hamstring tendon grafts exceed the strength of a normal ACL. The bottom line is 85% to 95% of patients will have clinically stable knees following ACL reconstructive surgery.
Post-Surgical Rehabilitation of the ACL
Post-surgery, rehabilitation should begin immediately. Post-surgery priorities include avoiding disruption of the wound healing and encouraging full knee extension. Continuous passive motion can be used to help with decreasing effusion in the knee. It is extremely important for the supervised rehabilitation to be supplemented by a home fitness program prescribed by your therapist.
Important abnormal post-operative signs to monitor:
- unusual erythema and effusion
- abnormal pain response
- lack of 90 degrees of knee flexion by post-operative day 10
All athletes will undergo a 6-month post-operative rehabilitation that can be divided into 6 phases. Return to activity requires both time and clinic evaluation. To efficiently return to normal or high-level functional activity, the athlete requires adequate strength, flexibility, and endurance.
Too see a detailed breakdown of the 6 phases of the 6 month rehabilitation program we employ at Back to Function, please see the article Post-Surgical Rehabilitation of the ACL.
If you have a knee issue that needs to be evaluated, please give us a call at 310-534-1900 or email us at info@backtofunction.com.
Massachusetts General Hospital, Sports Physical Therapy Program. Rehabilitation Protocol for ACL Reconstruction.
University of Wisconsin Sports Medicine. Rehabilitation Guidelines for ACL Reconstruction in the Adult Athlete (Skeletally Mature)
Baylor College of Medicine, Sports Medicine. Anterior Cruciate Ligament Reconstruction Accelerated Rehab.
ACL Return to Sport Guidelines and Criteria. Davies, George J, McCarty, Eric, Provencher, Matthew, Manske, Robert. 2017 Sep: 10(3): 307-314.
ACL Rehabilitation Progression: Where Are they Now? Cavanaugh, John, Powers, Matthew. 8 Aug 2017. Curr Rev Musculoskelet Med (2017).
ACL Reconstruction Rehabilitation: A Systematic Review Part 1. National Institutes of Health. 2008 July; 21(3): 217-224.


